Integration of Chinese and Western Medicine - From Experience to Evidence-Based Medicine
Prof. Justin WU
Associate Dean((Development), Faculty of Medicine, The Chinese University of Hong Kong
Professor of Department of Medicine and Therapeutics
Founding Director of Hong Kong Institute of Integrative Medicine (HKIIM), Faculty of Medicine, CUHK
Host: Ms Janet Wong
Information Compilation : Ms Vivien Kam
Ms Bernadette Cook


Introduction:
In recent years, more and more people have become interested in the combination of Chinese and Western medicine in cancer treatment. Professor Justin Wu is a gastroenterologist on the one hand, and the founding director of Hong Kong Institute of Integrative Medicine (HKIIM), Faculty of Medicine, CUHK on the other. In this interview, he shares his views on the combination of Chinese and Western medicine in cancer treatment, especially the recent developments in scientific research.
Part One - Background of the Establishment of the Hong Kong Institute of Integrative Medicine (HKIIM), Faculty of Medicine, CUHK
Part Two - Service Scope of the Hong Kong Institute of Integrative Medicine (HKIIM), Faculty of Medicine, CUHK
Part Three - Differences and Similarities between Chinese and Western Medicine: Using Gastrointestinal Diseases as an Example
Part Four - Scientific Research on the Combination of Chinese and Western Medicine
Part One - Background of the Establishment of the Hong Kong Institute of Integrative Medicine (HKIIM), Faculty of Medicine, CUHK
Wong: Professor Wu, thank you very much for accepting our interview today to talk about the background and current work of the establishment of the Hong Kong Institute of Integrative Medicine (HKIIM), Faculty of Medicine, CUHK (hereinafter referred to as the "Institute"). At the same time, you are a gastroenterologist, and I would like to ask you about the possibility of combining Chinese and Western medicine in the field of gastroenterology.
Wu: You're most welcome.
Wong: As far as I understand , the Chinese University established this Institute in 2014. It is the first clinic in Hong Kong to be jointly managed by Chinese and Western medical professors, providing Chinese medicine, Western medicine and integrated Chinese and Western medicine treatment. I know that you were the founding director of the Institute at that time. May I ask what was the philosophy behind the establishment of this Institute by the Chinese University at that time?
Wu: Traditional Chinese medicine has a long history and is particularly effective in treating certain diseases. As Western doctors, we understand that there are limitations in the treatment of some diseases in Western medicine, such as how to alleviate some chronic diseases and pain management. I myself am a gastroenterologist, and irritable bowel syndrome (IBS) is an example.
At that time, we wanted to establish a center for the integration of Chinese and Western medicine, composed of professors of Chinese medicine, professors of Western medicine, specialist doctors, registered Chinese medicine practitioners, and nurses etc., committed to clinical services and actively participating in medical research, training, and teaching.
Therefore, the Chinese University established this Institute in 2014. Our key areas include: chronic diseases, pain management, geriatric frailty, rehabilitation, etc.

Part Two - Service Scope of the Hong Kong Institute of Integrative Medicine (HKIIM), Faculty of Medicine, CUHK
Wong: Can you give us an introduction to the services the Institute currently provides?
Overview
Wu: The medical services provided by the Institute cover Chinese medicine general practice, pain, metabolic diseases, cancer, etc., as well as acupuncture and orthopedic services.
In terms of Western medicine, it also provides family medicine, pain management, etc. The Institute is currently expanding its integrated Chinese and Western medicine treatment plans for cancer treatment, stroke rehabilitation, and back pain, and is committed to building a safe and high-quality integrated Chinese and Western medicine treatment platform.

Cancer Treatment
Wong: This handbook is written for caregivers of cancer patients, so I am most concerned about cancer treatment. Can you talk to us about the development in this area?
Wu: Cancer treatment is one of the service areas of our Institute. Perhaps I should first explain how we set the priority of services when our Institute was established.
Western medicine and Chinese medicine have always developed along different philosophies and systems. We know that building a bridge between Western medicine and Chinese medicine is not an easy task. So after careful consideration, we decided to focus on projects that are easier to see results and are not controversial.
Cancer is a very serious disease. The concept of Western medicine is to use different methods to eliminate cancer cells, such as surgical removal, radiation therapy, and chemotherapy, and targeted therapy and immunotherapy that have been actively developed in recent years are also in this direction. However, these treatments all have their limitations. Although they can completely or partially eliminate cancer cells, patients also have to suffer different side effects after treatment. Some side effects are well managed by Western medicine, but some face many limitations.
Everyone knows that after chemotherapy, patients often have side effects, such as vomiting, oral ulcers, loss of appetite, etc. In Western medicine there are not completely effective treatment methods. So we hope to use Chinese medicine to complement Western medicine treatment, to provide patients with better overall treatment.
At the same time, if the cancer has reached a very late stage, and Western medicine has no treatment plan to offer to the patient; or if the patient is too old and weak to accept Western medicine treatment, then Chinese medicine can provide another option.
Furthermore, in pain management, Western medicine has recognized that acupuncture is effective. This is also an area we value.
Wong: I totally agree. In providing complementary reatment, symptom management, and palliative care, Chinese medicine definitely has its role. Especially when the cancer has reached an uncontrollable stage, doctors will honestly tell the patient that they have nothing more to offer. So there is no dispute about patients trying out Chinese medicine treatment.
May I ask Professor, is Chinese medicine mainly focused on the "complementary " aspect in treating cancer, that is, improving the patient's constitution, strengthening the foundation and nourishing the origin(固本培元), rather than "actively fighting cancer", that is, directly killing cancer cells?
Wu: I think it's both.
The basic concepts of Western medicine and Chinese medicine in treating cancer are different. Western medicine aims to eradicate cancer cells, but Chinese medicine believes in "holistic" treatment. The philosophy of Chinese medicine is that a person gets sick because there are different problems in the body - it can be due to external factors, the so-called "external evil invasion"(外邪); or there is a problem with the body itself. So the main method of Chinese medicine in treating cancer is "strengthening the body and expelling the evil", strengthening the patient's body in all aspects. For example, as long as the patient eats better, sleeps better, and lives more comfortably, it is already a great help.
However, some Chinese medicines may really contain some chemical components that can cause cancer cells to slowly die, which has an anti-cancer effect.
In fact, whether it is to strengthen the patient's physique or to cause cancer cells to die, the hope is to help patients in the fight against cancer tilt the balance, not to let cancer cells grow unceasingly and advance, until the patient dies.
Wong: Very often when patients are undergoing Western medicine treatment, they see Chinese medicine practitioners at the same time, but they are worried that this will offend the doctor.
Wu: Different doctors have different views on Chinese medicine treatment. Some doctors will tell patients that they neither encourage nor oppose it, because they do not understand it. This is not unreasonable, because as doctors they should not provide opinion on things they do not understand.
But now more and more doctors are open to Chinese medicine treatment, they will analyze with patients, especially if a certain cancer has no way to treat from a Western medicine perspective, then what's the harm in trying out Chinese medicine treatment?
Wong: If accepting Chinese medicine treatment does not affect Western medicine treatment, that would be the best. But if there are some situations where Chinese medicine treatment and Western medicine treatment contradict each other, how should the patient choose?
For example, a patient with pancreatic cancer: Western medicine suggests that he undergoes Whipple Operation, but his Chinese medical practitioner opposes surgery, believing that it will "break the qi" (破氣)or disrupt the internal organs, persuading the patient not to have surgery, and purely accept Chinese medicine treatment. Then the patient will be very hesitant, not knowing what to do.
Under such circumstances, what is your suggestion?
Wu: As a Western doctor, I can't exactly understand the effectiveness of the treatment method suggested by the Chinese medicine practitioner. But I can analyze in detail with the patient what Whipple surgery is, what the goal of the surgery is, what the risks are, the success rate, and prognosis, etc.
During the explanation process, I will provide appropriate statistical data. For example, we will honestly tell the patient that at this stage if he accepts the surgery, according to statistics he should have about two years of survival time; ask him to consider what these two years mean to him. At the same time, we will tell him what the foreseeable consequences are if he does not accept this surgery.
My goal is to let the patient understand his situation as much as possible, and make a decision that he thinks is most suitable for him.
This is the spirit of evidence-based medicine.
Part Three - Differences and Similarities between Chinese and Western Medicine: Taking Gastrointestinal Diseases as an Example.
Wong: Professor, you are a gastroenterologist, I would like to ask you: How do you understand and treat the same gastrointestinal problem from the perspective of Western medicine and traditional Chinese medicine? For example, we Chinese often say that eating a lot of fried food or lack of sleep, the next day will have "heat"(熱氣), gastrointestinal discomfort and bad breath. What is the reason for this from the perspective of Western medicine? And what is the reason from the perspective of traditional Chinese medicine?
Wu: From the perspective of Western medicine, we have different bacterial groupings in our intestines, and the types and quantities of these bacterial groupings directly affect our gastrointestinal health and even our overall health. If a person lacks sleep, is under emotional stress, or eats unhealthy food, it will affect the ecology and balance of the intestinal bacteria and cause mild inflammation. If a person's gastrointestinal tract is inflamed, it will produce a smell and the smell will leave the body through exhalation, which is bad breath.
From the perspective of traditional Chinese medicine, it is the imbalance of the spleen(脾), leading to "fire"(火), "heat"(熱氣), etc. Then traditional Chinese medicine will regulate the gastrointestinal function for the patient, "reduce fire"(降火), and solve the problem for the patient.
So although different vocabulary is used, there are commonalities in fact.
Wong: So how would Western medicine and traditional Chinese medicine treat this problem?
Wu: From the perspective of Western medicine, since the patient has mild inflammation, we will give him appropriate medication to reduce inflammation and thus achieve the purpose of cure.
From the perspective of traditional Chinese medicine, they will give the patient some Chinese medicine to "clear the heat"(清熱). In fact, many herbs are polysaccharides, they all have their unique chemical substances, and after entering the intestines, they will cause some changes in the bacterial groupings, improving the patient's condition.
So if we analyze in detail, we will feel that Chinese medicine makes very good sense. It's just that Western medicine and traditional Chinese medicine do not have a good bridge to understand each other and complement each other.
Wong: Both are really ingenious in their own ways.
So what about "cold"(寒)?
Wu: From the perspective of traditional Chinese medicine, they have what is called "stomach cold"(胃寒), the symptom is that the patient has poor digestion and stomach discomfort. Traditional Chinese medicine sometimes tells patients to eat some ginger to "warm the stomach"(暖胃), and often the patient's condition will improve after eating.
From a Western medical perspective, we believe that the patient's problem stems from having too much of a certain chili enzyme (Chilli receptor) in his intestines. People with this enzyme are very sensitive to certain chemicals, and as soon as the patient eats a small amount of food containing these chemicals, his alarm system will be stimulated to "misfire", causing discomfort in his stomach. Western medicine will give the patient some low-dose chili enzymes to gradually adapt his stomach, which is to desensitize (reduce sensitivity) or regulate these receptors.
Wong: So taking Chinese medicine can change the ecology within our bodies through its unique chemical composition , thereby achieving therapeutic effects?
Wu: Yes. Chinese medicine can affect various aspects of the body - including metabolism, blood circulation, etc. Some people say they feel that taking Chinese medicine is useless or has no effect on the body. I laugh and say, "Try putting ten different kinds of Chinese medicine into your stomach and see if it has an effect. There is definitely an effect, but I don't know if it's a good effect or a bad effect."
Wong: I remember many years ago, I took some Chinese medicine given to me because I was feeling unwell. I don't remember if it was Isatis root or San Dong tea: after drinking it, I felt uncomfortable all over and even fainted. What actually happened?
Wu: I can't fully explain. But one possibility is that the Chinese medicine you took had a strong effect, which could reduce some inflammation in the body, or stimulate the immune system. You took so much Chinese medicine that day, it might have led to what Western medicine calls a cytostorm - the immune function in the body is affected, even disordered, leading to the situation at that time.
Wong: I see.
I know some people have a disease called Irritable Bowel Syndrome, where patients will have bloating, stomach pain, diarrhea, etc. So how do Western and Chinese medicine view this disease?
Wu: From a Western medical perspective, Irritable Bowel Syndrome can be related to a person's emotions, so sometimes the more nervous you are, the bigger the problem. From a Chinese medicine perspective, many diseases, including Irritable Bowel Syndrome, are also related to emotions, which is the so-called "emotional state".
So Western medicine refers to it as "stress"; Chinese medicine refers to it as "emotional state"(情志). Western medicine will prescribe drugs to patients in hopes of solving emotional, insomnia and other problems, thus treating irritable bowel syndrome. Chinese medicine, on the other hand, will help patients "calm the mind" and "relieve stress". Everyone's view is that psychology affects physiology, but the vocabulary used is different.
We are currently researching an ancient formula with the Baptist University, which contains seven kinds of Chinese medicine. We hope to understand how these drugs can affect a person's physiological condition, especially the gastrointestinal system. Two years ago, we received approval from the China Drug Administration and are now conducting clinical research.

Part Four - Scientific Research Combining Chinese and Western Medicine
Wong: We just talked about "evidence-based", which is a very important concept and is very important in scientific research. I understand that your Institute also conducts scientific research. The tradition of Chinese medicine has always been based on experience, and it is not as strong as Western medicine in evidence-based medicine, as it cannot provide accurate and objective data like Western medicine. How would you handle this?
Wu: In terms of evidence-based medicine, Chinese medicine is indeed not as strong as Western medicine in terms of "quality" and "quantity". Therefore, when we established this Institute, one of our concepts was to push the research of Chinese medicine towards evidence-based medicine.
About ten years ago, I met an old Chinese medicine practitioner. He received Chinese medicine training in the Mainland when he was young, and then went to Australia to study Western medicine, so he has a thorough understanding of the theories of Chinese and Western medicine. Later, he practiced in Hong Kong and set up his own Chinese medicine clinic. Many of his patients are cancer patients.
After we got to know each other, we often discussed how to treat gallbladder, pancreas and rectal cancers. As I just said, the treatment method of Western medicine is to eliminate cancer cells; but Chinese medicine believes that all cells are from our own body, but only a part is affected by "evil"(邪). If the body can be successfully "supported", the patient can resist cancer, and even if it cannot recover, it can "coexist with cancer"(與癌並存).
This Chinese medicine practitioner has a very open attitude. He allowed us to analyze his records, knowing what diseases the patients had, the conditions when the disease occurred, what Western and Chinese medical treatments were received, and the results, etc. This information is very valuable, allowing us to systematically summarize and analyze.
At the same time, we also study his prescriptions in detail, look for the trajectory of treatment, and conduct correlation analysis of the disease and treatment results. Our long-term vision is:
- We hope to know what kind of traditional Chinese medicine can treat what kind of disease:
- Further analyze the main medicinal ingredients (active ingredients) of individual Chinese medicines. If they can be proven to have therapeutic effects, they can be used as the basis for drug development in the future. This is the application of academic research results in the real world (realisation of academic research); and
- In addition to treatment, if we can find that some Chinese medicine ingredients can prevent some cells in the body from inflammation or disease (and these changes, if not stopped, can lead to colon cancer in the future), we can reduce the incidence of colon cancer by preventing these inflammations/diseases. This can open up a new field in the prevention of cancer by combining Chinese and Western medicine.
Wong: In the scientific research of combining Chinese and Western medicine, what do you think is the most difficult part?
Wu: Western medicine and Chinese medicine are two completely different systems. We want to use one system to verify another system; or use one ruler to "measure" another ruler, which is not without difficulty.
Now we are using the ruler of Western medicine, hoping to understand the mystery of Chinese medicine treatment systematically based on this.
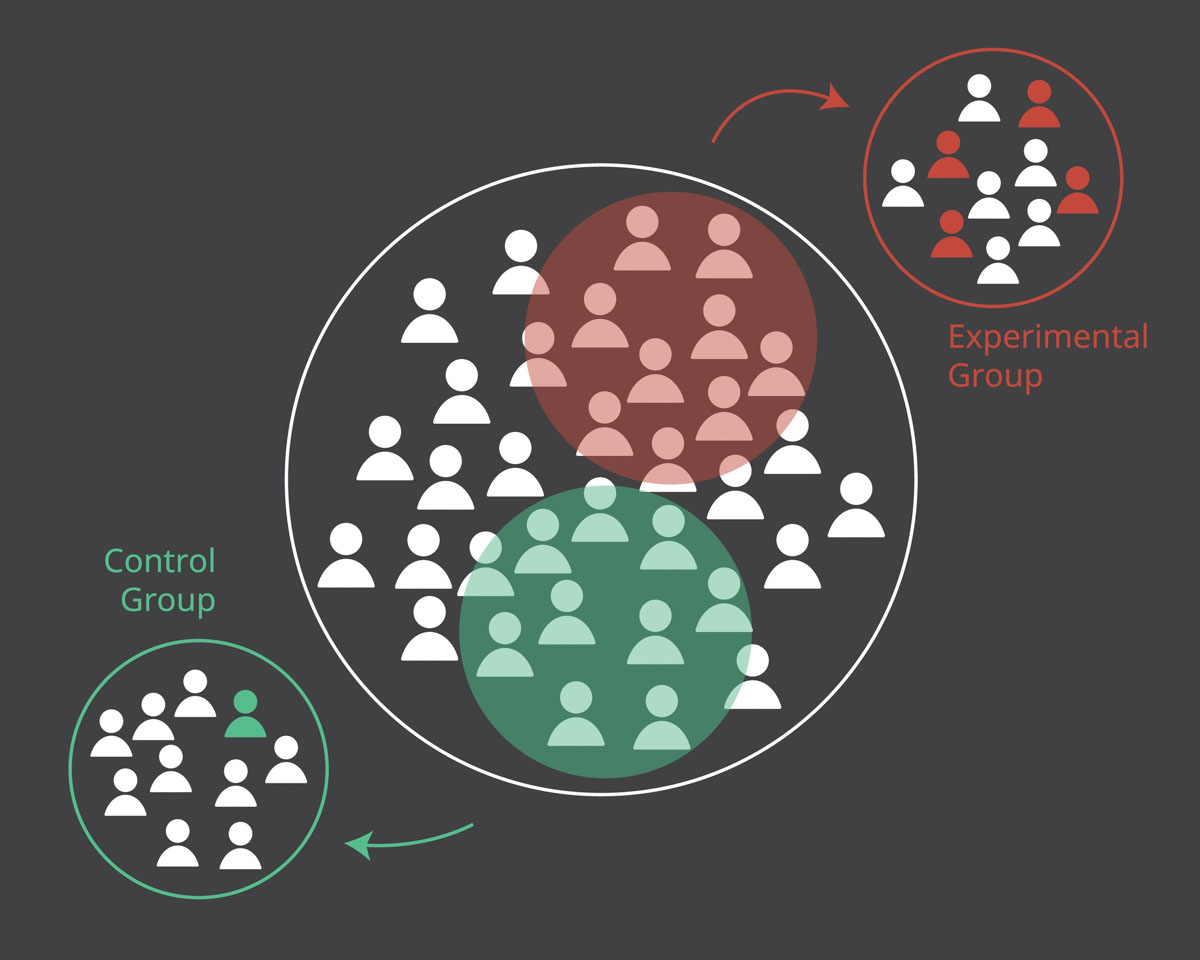
If we come up with some theories through research in the future, we can conduct double-blind randomized controlled trials to verify the efficacy of Chinese medicine.
Wong: This is very interesting! But it requires a lot of manpower, resources, and time.
Wu: Yes. However, the emergence of artificial intelligence and big data has opened up a new world for our scientific research.
In recent years, their rapid development has given the medical community unprecedented strong analytical capabilities. We have the ability to conduct detailed analysis of the statistics on different elements (such as the patient's condition, different treatments received at different times, treatment results, etc.). Through these processes, we can decipher whether there is a relationship between certain elements, and if so, what is the relationship.
Now you will hear a lot about OMICS, including Metaomics (research on metabolism), Genomics (research on genes), etc., which have developed well due to the emergence of big data.
The old Chinese medicine doctor I mentioned to you earlier, when he immigrated, he donated all his records to the Chinese University as research materials, which is very useful and precious to us.
We are just starting now, but we hope to do more and more in the future, and to do it on a larger scale.
Wong: I am very grateful to you, Professor, for accepting my interview today, which has deepened our understanding of the topic of the integration of Chinese and Western medicine.
Wu: You're welcome.
(December 2021)